Emily Scarr
State Director, Maryland PIRG; Director, Stop Toxic PFAS Campaign, PIRG
State Director, Maryland PIRG; Director, Stop Toxic PFAS Campaign, PIRG
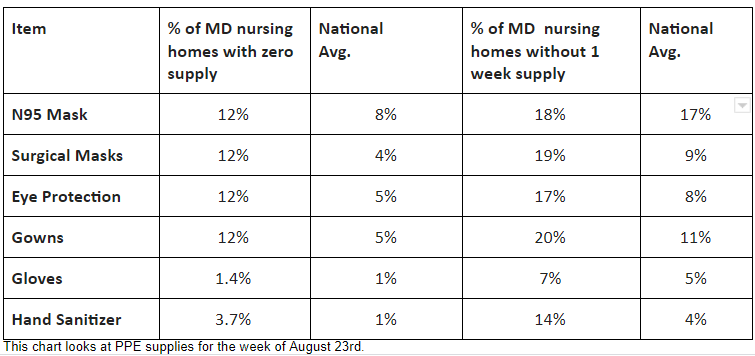
Baltimore — Maryland nursing homes, along with thousands nationwide, have horrific shortages of masks, gowns and other items they need to protect residents, workers and the broader community from COVID-19. When nursing homes don’t have enough personal protective equipment (PPE), it can lead to outbreaks among residents and staff, worker quarantines and shortages, and more risk to workers’ and residents’ families and neighborhoods.
Maryland has had more than 2,000 deaths from residents and staff at nursing homes, group homes and assisted living facilities, which accounts for more than half of the confirmed COVID-19 deaths in the state.
“It’s outrageous that we are dealing with severe PPE shortages seven months into the pandemic, especially in our nursing homes where some of the most vulnerable members of our community members.” said Emily Scarr, Maryland PIRG Foundation director. “Without proper PPE nursing home cases can spread rapidly, putting others at risk inside and outside the facility.”
In the spring, outbreaks in nursing homes made state and national headlines. Now, seven months into this pandemic, PPE shortages have become much worse, according to “Nursing home safety during COVID: PPE shortages,” a report by Maryland PIRG Foundation and Frontier Group. Our analysis of data submitted to the Centers for Medicare & Medicaid Services by the nation’s 15,000 nursing homes, and 220 in Maryland, shows that Ad:
“I’m most shocked that the number of nursing homes out of PPE actually tripled between July and August. We can and must do better,” Scarr said.
Scarr added that experts believe PPE shortages have continued to get worse. One group, GetUsPPE, a grassroots movement founded by medical professionals on the COVID frontlines, said more facilities across all sectors were complaining of shortages in September.
“Having less-than-one-week supply is regarded as a critical shortage in our industry. It’s considered the minimum acceptable. If a home has an outbreak, we can burn through a limited supply in a day or two,” explained Katrina Johnson, a Maryland Nursing home worker.
“A nursing home may have no idea when its next shipment of PPE may arrive. Homes with less than one week’s supply often ration, forcing workers to re-use PPE or go without,” explained Donta Marshall, Vice President 1199SEIU. “We need to do much better to protect the residents and staff of Maryland’s nursing homes and the communities around them.”
Medical experts believe the shortage of PPE is a key reason that outbreaks and deaths from COVID-19 are disproportionately high in nursing homes. In Baltimore, the Maryland Baptist Home has received national attention for their work to protect their residents from the virus, and their ability to stock up on PPE was a crucial factor in their success.
This issue becomes even more urgent with talk of a herd immunity strategy that would allegedly safely cordon off nursing home residents and other at-risk populations while COVID tears through the rest of society. In reality, evidence suggests that until we have a vaccine, without a stronger adherence to spread-prevention practices that usually involve PPE, infection will likely run rampant.
In the report, Maryland PIRG Foundation calls for a number of policy actions to improve the supply and transparency of availability of PPE. These actions include: the federal government fully implementing the Defense Production Act so more PPE is available and sold at reasonable prices; congressional action to streamline the supply chain; and multi-state consortiums to reduce competition and stabilize prices.
The PPE shortage is among the problems brought to light by the data on nursing homes. We will explore various issues in a series of reports in the months ahead.
View our guide: “20 questions to ask your nursing home during COVID.”
****
Maryland PIRG Foundation is an independent, non-partisan group that works for consumers and the public interest. Through research, public education and outreach, we serve as counterweights to the influence of powerful special interests that threaten our health, safety or well-being.